This is borderline unbelievable, with staggering implications for our wounded. A company called RHTRLLC has developed a Bio-Electric Wound Dressing that basically cuts the healing time for surface injuries in half.
Yes, in half.
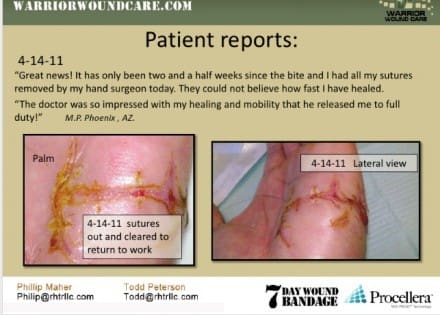
They call it the 7 Day Wound Bandage, and it’s really interesting stuff. There were pictures and case studies there showing the positive results of bioelectric bandaging on everything from burns to injuries suffered by a man that went through the windshield of his car to a case of facial cancer. All of them benefited from the use of the bandage, which is essentially a lightweight piece of cloth covered in tiny, wafer thin disks of different metal activated upon application to provide a very mild electric current that speeds healing.

It’s not just big injuries in the hospital that benefit, either. One of the guys at their booth developed blisters walking around SHOT. He pulled a couple of these patches from his wallet, put ‘em on his heels and was substantially improved by the next day. A sheriff’s deputy working along the border related that he’d been tagged by a scorpion (a very painful sting, as some of you may know first hand) and was able to remain in service after putting one of these bandages on the sting’s location. Another story—this one something you grunts will relate to—involved your basic case of crotch rot. On a hump at a training day, the individual concerned developed raw, painful skin on his thighs and perineum. He threw some 7 Day Bandage on there and believe it or not was soon able to walk without looking like some mutant from a SyFy movie.
This is a quote from a study conducted at a Burn Center involving the use of bioelectric dressings:
______________________________________________________________________
Abstract Title: Use of Bioelectric Dressings for Faster Wound Healing: A Prospective Case Series
Authors: Andrew Blount, MD; Sarah Foster, MD; Richard Wilcox, MD
Blodgett Hospital Burn Center, Grand Rapids, MI
PURPOSE
Despite advancements in wound care treatments for the management of acute and chronic wounds, there is an unmet need for interventions that accelerate epithelialization. Recent research findings support the use of bioelectric wound dressings to address this challenge (1-3). The principal aim of this study is to evaluate the impact of a bioelectric wound dressing on acute wound healing
METHODS
Thirteen participants presenting to a multidisciplinary burn clinic were enrolled. Each patient underwent split-thickness skin graft (STSG) for treatment of their burn wound, with their donor site serving as the wound addressed for this study. STSG donor sites are the ideal control wound as they are of relatively uniform depth and have square margins for simple application of dressings. Each participant serves as his/her own control; one half of all wound sites were treated with the bioelectric dressing and semi-occlusive dressing, the other half using solely semi-occlusive dressing (SOD). At each standardized follow-up visit, percent epithelialization and scar quality of wounds was rated by the same attending burn surgeon who served as a blinded evaluator. Localized pain was recorded using a Numeric Pain Intensity Scale. At monthly follow-ups, participants provided a self-assessment of their scar appearance.
RESULTS
At week 1 post-procedure, average epithelialization of 64.2% (SD=34) was noted on the bioelectric dressing treated side, compared to 46.9% (SD=33) on the SOD side, representing an average 36.89% faster wound healing (p=.028). At one month, patients
rated the bioelectric dressing treated half superior in terms of color, thickness, and overall quality (p<0.05, two-tailed).
CONCLUSION
This early data shows promise in terms of faster healing, improved scarring, and
improved patient outcome with the use of the bioelectric dressing on acute wounds. With fulfillment of an extended study population, we hope to provide a solid foundation for extrapolating our data beyond skin graft donor sites to all areas of wound care.
______________________________________________________________________
For more information, contact Todd M Peterson, RHTR LLC, todd@rhtrllc.com,
www.warriorwoundcare.com.
-DR
Tags: 7 Day Wound Bandage





If accurate that is pretty staggering. I hope it is true.
It is true. I know the guys who own it and they have been pushing since 08 to get into the hands of the US Military. Politics and BS are keeping it out of our IFAKs.
No, the fact that this was developed for definitive care use and not field use is what’s keeping it out of the IFAK. It does nothing to slow or stop bleeding and doesn’t belong in a trauma kit. For longer term use once the wound has been debrided, cleaned, etc etc, certainly. But the verdict is still out on efficacy and long-term use. Very little research has even been published on this product and all the studies that I’ve managed to find so far have been paid for by Vomaris, the company that actually developed the Procellera bandage. Anecdotes are all fine and well, but when it comes to medicine, I prefer hard science.
Then perhaps someone at a MEDCEN needs to get off their wide ass and test it.
Oops, sorry, meant to type “procellera dressing”, not “bandage. Mea culpa!
I am really intrigued by this product and what it could mean for getting troops back into the fight after an injury, however, I agree with Ian, it does not belong in the IFAK; that space is reserved for immediate, life-saving interventions. This product would be great to get in the hands of the BAS medics back on the FOB where injuries can be cleaned an properly analyzed, etc., but for field use, I don’t see it being practical. Definitely believe there is a use for it in the military though, just has to be right time and place.
Actually Ian, there are several independent studies that show these dressings really do work… as well as tests within the military. The dressings have NSNs, order some and try them yourself.
We have gone down this road on this dressing. We’ve found that while it is a dressing, and it does work as a dressing, its efficacy is no better than clean bandages, silverlon, or any other dressing/bandage capacity that it’s competing against. This is why it hasn’t taken off as the new way ahead in dressings. The NSN is for an HA application…not for trauma, burns etc. If anyone has NEW hard data on these, let us know.
Looks like this needs a lot more testing – those standard deviations are pretty terrible for a performance-oriented report (where’s the explanation on how it works in the method? How is this chemically induced?). Nevertheless this looks like a really promising product; I particularly like the repair of lost tissue on the lower lip of the child, and how it was replaced in such a short period of time with negligible scarring.
IFAK, whatever. If you say only immediate care stuff belongs in the IFAK then why the hell does mine come with band aids and iodine tablets? If it works, then it works. A trauma kit is different than a first aid Kit. Doesn’t the soldier sustain injuries in the field that are not immediately life threatening like blisters or ruck sores ? How about that thing on his lip that he got in Thailand? I’m guessing band aid paid for their own testing too. I wouldn’t sit around and wait for a government that can’t approve their own budget to test my product if it could be helping people right now.
Guerrilla, I think I have stuff in my aid bag for the non-life threatening injuries guys sustain in battle. I wouldn’t ask my guys to carry all their own band aids and moleskin and whatever else they may need. I could maybe see the iodine tablets, but I can’t imagine why your IFAK has bandaids (or why mine has gloves for that matter). When it comes to putting extra weight on my guys’ kit, I won’t ask them to carry anything that’s not going to be used as a life-saving intervention; that’s my job.
Here is what the issue IFAK has in it.
(1ea) Pouch NSN 8105-09-000-2725
IFAK A1 Component Individual First Aid Kit – NSN 6545-01-539-2740 (includes the following items):
(1ea) 3.5 oz. Quikclot Packet – NSN 6510-01-499-9285
(2ea) TK4 Tourni-Kwik Self-Application Tourniquet 40″ – NSN 6515-01-542-7696
(2ea) “H” Compression Bandage w/8″ x 10″ Ab Pad – NSN 6510-01-540-6484
(2ea) Primed Compressed Gauze 4.5″ x 4.1 yards – NSN 6510-01-503-2117
IFAK A1 Minor First Aid Kit Component NSN 6545-09-000-2727 (includes the following items):
(5ea) Adhesive Bandage 2″ x 4 1/2″ – NSN 6510-01-514-4518
(10ea) Adhesive Bandages, 3/4″ x 3″ – NSN 6510-00-913-7909
(2ea) Triangular Bandages, 40″x40″x56″ Non-sterile – NSN 6510-00-201-1755
(1ea) Combat Reinforcement Tap 2″ x 100″ – NSN 6510-01-549-0927
(1ea) Burn Dressing 4″ x 16″, Water-Jel – NSN 6510-01-243-5894
(8ea) Bacitracin Antibiotic Oinment 0.9 gram
(1ea) Povidone-Iodine Topical Solution USP 10% 1/2 floz. – NSN 6505-00-914-3593
(1ea) Water Purification Tablets 10 Pack, Katadyn Micropur, Sodium Chlorite – NSN 6850-00-985-7166
I don’t understand where this topic is going or how it became a debate on who decides what goes into an IFAK. My point is this, that dressing works, and everyone should have it. Thats my opinion .