RESEARCH TRIANGLE PARK, N.C. — New U.S. Army-funded research demonstrates a connection between stress and stomach ulcers.
The research, conducted at the University of Pittsburgh Brain Institute and funded by the Army Research Office traced neural pathways that connect the brain to the stomach, providing a biological mechanism that explains the connection.
ARO is an element of the U.S. Army Combat Capabilities Development Command’s Army Research Laboratory.
“The bidirectional connections between brain and gut are important conduits for communication within the mind-body axis,” said Dr. Frederick Gregory, ARO program manager. “The biological mechanisms into how stress might influence cognitive performance plays a central role in future strategies to mitigate Soldier stress through diet or other new gut-centric interventions. Not only is this important for combat missions but for the overall health and well-being of the entire Army.”
The findings, published this week in the Proceedings of the National Academy of Sciences, build a scientific basis for the brain’s influence over organ function and emphasize the importance of the brain-body connection.
Until now, research exploring the gut-brain interaction has largely focused on the influence of the gut and its microbiome on the brain and neurological disorders. But it’s not a one-way street – the brain also influences stomach function.
“Pavlov demonstrated many years ago that the central nervous system uses environmental signals and past experience to generate anticipatory responses that promote efficient digestion,” said Peter Strick, Ph.D., Brain Institute scientific director and chair of neurobiology at Pitt. “And we have long known that every increase in unemployment and its associated stress is accompanied by an increase in death rates from stomach ulcers.”
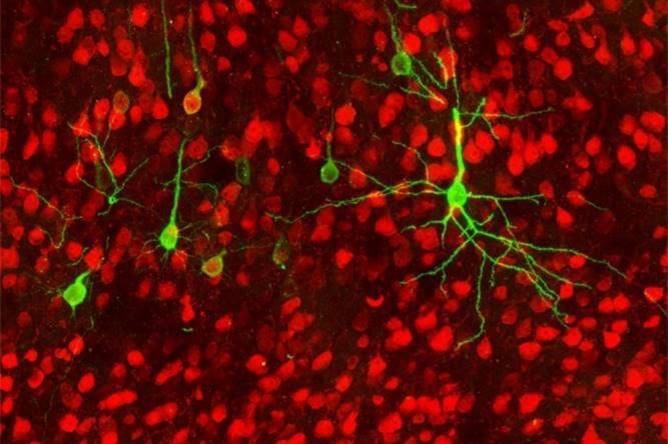
To find brain regions that control the gut, Strick and his coauthor David Levinthal, M.D., Ph.D., assistant professor of gastroenterology, hepatology and nutrition at Pitt, used a strain of rabies virus to track connections from the brain to the stomach.
After being injected into the stomach of a rat, the viral tracer made its way back to the brain by hopping from neuron to neuron – using the same trick that rabies virus uses to infiltrate the brain after entering the body through a bite or scratch – to reveal the brain areas that exert control over the stomach.
The researchers found that the parasympathetic – rest and digest – nervous system pathways trace back from the stomach mostly to a brain region known as the rostral insula, which is responsible for visceral sensation and emotion regulation.
“The stomach sends sensory information to the cortex, which sends instructions back to the gut,” Strick said. “That means our ‘gut feelings’ are constructed not only from signals derived from the stomach, but also from all the other influences on the rostral insula, such as past experiences and contextual knowledge.”
In contrast, the sympathetic – fight or flight – pathways of the central nervous system, which kick in when we’re stressed, predominantly trace back from the stomach to the primary motor cortex, which is the seat of voluntary control over the skeletal muscles that move the body around.
Identifying these neural pathways that connect the brain and stomach could provide new insights into common gut disorders.
For example, Helicobacter pylori infection typically triggers ulcer formation, but descending signals from the cerebral cortex could influence the bacteria’s growth by adjusting gastric secretions to make the stomach more or less hospitable to invaders.
These insights could also change clinical gastroenterology practice. Knowing that the brain exerts physical control over the gut gives doctors a new way to approach bowel problems.
“Several common gut disorders, such as dyspepsia or irritable bowel syndrome, might not get better with current treatments,” said Levinthal, who is also a gastroenterologist at UPMC. “Our results provide cortical targets that will be critical for developing new brain-based therapies that might be helpful for our patients.”
Gregory said that this is particularly relevant to combat casualty care where there are often bowel problems such as traveler’s diarrhea that can affect the overall health and performance of the military.
In addition to the U.S. Army, the National Institutes of Health and the DSF Charitable Foundation supported this work.
By U.S. Army CCDC Army Research Laboratory Public Affairs


It took research to figure out what they be known since I was a kid?
And in breaking news, water is indeed wet! More at 11.
Leave it to bureaucracy to waste who knows how much money on research to arrive at a conclusion that’s been common knowledge for decades.
I figured someone would get the irony in this.
You are joking right?
The folksy wisdom of “ulcers are CAUSED by stress” has been disproven. In the 1980s, Dr Barry Marshall was laughed at for his research and hypothesis that ulcers were caused by bacteria. He went so far as to infect and then cure himself (h. pylori is the bacteria). In 2005 he and others were awarded the Nobel Prize for this work, and it’s links to gastritis and stomach cancers.
The link (NOT cause) between an ulcer and stress has remained in public consciousness and assumption- however this and every other study are critically important to an actual scientific understanding of mechanism vs exacerbating factors or comorbidity.
The PROVEN (not assumed) link between gut health and brain function is recent, and this study showing a CAUSAL (not associated) link, a defined mechanism- is very important and has wide ranging implications.
An observed link between stress and ulcers is not the same as determining a mechanism. Nor does this follow the old line of “relax, you are going to get an ulcer”, there is a hell of a lot more going on here.
This is useful science, not in any way a bureaucratic waste.