The Air Force Research Laboratory’s cutting-edge research creates future warfighting technologies for the Air and Space Forces, protecting the lives of those that put themselves in harm’s way. Ground-breaking research into cellular reprogramming, made possible in part with funding from AFRL’s Air Force Office of Scientific Research, is leading to technology that could heal wounds more than five times faster than the human body can heal naturally, vastly improving long-term health care outcomes for warfighters and veterans.
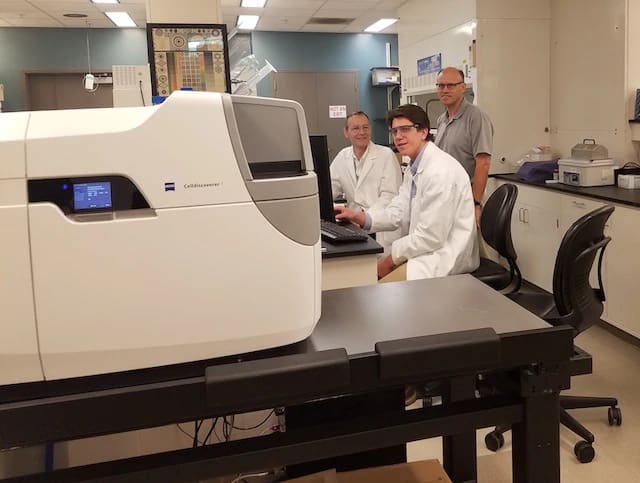
Dr. Indika Rajapakse, associate professor of Computational Medicine & Bioinformatics and associate professor of Mathematics at the University of Michigan, is researching ways to reprogram a person’s own cells to heal wounds faster. In order to get high-resolution views inside live cells to better understand the wound-healing process, Rajapakse submitted a Defense University Research Instrumentation Program proposal to purchase a live cell imaging microscope. Dr. Frederick Leve, program officer for AFOSR’s Dynamical Systems and Control Theory portfolio, selected Rajapakse’s proposal.
The microscope also assists in gathering data for an algorithm which can mathematically identify when best to intervene in a cell’s cycle to heal wounds. Leve, in collaboration with Dr. Fariba Fahroo, AFOSR program officer for the Computational Mathematics portfolio, awarded Rajapakse a grant for research to improve this algorithm.
“There are amazing opportunities in the United States, that you don’t see in the rest of the world, to humanize science and meet critical needs in medicine,” Rajapakse said. “We have the resources to do this, and it is our obligation to take full advantage of them. Thanks to the Air Force’s help, I was able to acquire the tools I need to advance my research into cellular reprogramming and wound healing.”
This funding connection was made possible by collaboration between the AFRL’s 711th Human Performance Wing, and Air Force Futures. Col. Charles Bris-Bois, the Air Force Disruptive Technology Team lead, was instrumental in making the connection between this novel technological concept and Air Force operational needs. The team saw a clear opportunity and helped Rajapakse reimagine his technology for other uses not immediately thought of such as aeromedical environments and how the presence of unhealed wounds increases aircrew susceptibility to hypoxia and other altitude related injuries.
“The impact of this research effort can be far reaching,” said Dr. Rajesh Naik, 711th Human Performance Wing chief scientist. “The convergence of biosciences with mathematical models can truly provide an inflection point to advance the development of wound healing. Dr. Rajapakse’s research can result in innovative solutions for addressing our needs in the aeromedical operations and in future space environments.”
Bris-Bois’ team used their real-world operational experience and insights to help uncover other potential challenge areas and medical applications, such as burn healing, skin grafts, organ transplants, etc. The continued partnership between AFRL and Air Force Futures helped to bridge the tech-to-operational divide, facilitating a move from the lab to real-world testing and applications.
“Indika’s research is exactly the kind of breakthrough technology we’re looking for in Air Force Disruptive Technology,” Bris-Bois said. “This shows the real promise of our efforts to bring warfighters and technologists together to imagine the possibilities of early scientific research.”
Cellular reprogramming is the process of taking one type of human cell, such as a skin cell, and reprogramming its genome so that it becomes a different kind of cell, such as a muscle cell, blood cell, neuron, or any other type of human cell. This is done using proteins called transcription factors. Transcription factors “turn on and off” various genes within cells to regulate activities such as cell division and growth, and cell migration and organization.
With the application of the right transcription factors, Rajapakse found that wounds healed more than five times faster than allowing the wounds to heal on their own. The next step is to figure out how best to apply them. The envisioned technology would act like a “spray-on” bandage, applying transcription factors directly to wounds. This method would convert exposed deep muscle cells into surface skin cells, which would mean a higher probability of successful healing than the current methods of skin grafting.
However, identifying which transcription factors make the required changes to create the right kind of cell requires a long process of trial and error. Rajapakse and his team have developed a data-guided algorithm to mathematically identify the correct transcription factors and predict the points in the cell cycle where transcription factors can best affect the desired change. The live cell imaging microscope provides data to further improve the algorithm.
“It’s rare that mathematics provides such promising results so quickly,” Leve said. “It usually takes decades for basic math research to make it into models which can be applied to a technology. In Dr. Rajapakse’s case, it only took a handful of years. AFRL is proud that our funding enabled mathematical theory for modeling and valuable data to be gathered which contributed to this rapid development.”
The success of Rajapakse’s project is a testament to AFRL’s purposeful outreach and relationships with partners such as Air Force Futures. This renewed commitment provides a mechanism for “out-of-the-box thinking” for potentially disruptive capabilities that will revolutionize the Air Force in the years to come.
“It is a really big deal that two opposite ends of the technology maturity spectrum — basic research and capability-focused operators — came together in this instance to identify an opportunity to help our warfighters and made it happen—fast!” said Dr. Shery Welsh, AFOSR director. “We are proud of our AFOSR Science and Engineering division for building an active, robust engagement with Air Force Futures that removed science roadblocks and created a pathway for transition.”
By Matthew D. Peters, Virginia Tech Applied Research Corporation


If the army really wants to get a return on investment, they need to focus on cartilage repair and regeneration.
Muscle and bone repair just fine, it’s spinal discs and knees that cause soldiers to leave. Unfortunately big army thinks it’s cheaper to pay VA disability for 30 years rather than invest in stem cell treatments for soldiers, but then disability payments doesn’t come out of the manpower budget now does it.
They could also do research on non-patentable healing peptides like tb500 or bpc157, the private sector is certainly not going to do it.