Qwick-AID Hemostatic Bandages feature no thermogenic reaction and maintain air permeability. Additionally, the bandage won’t stick to the wound and is hypoallergenic.
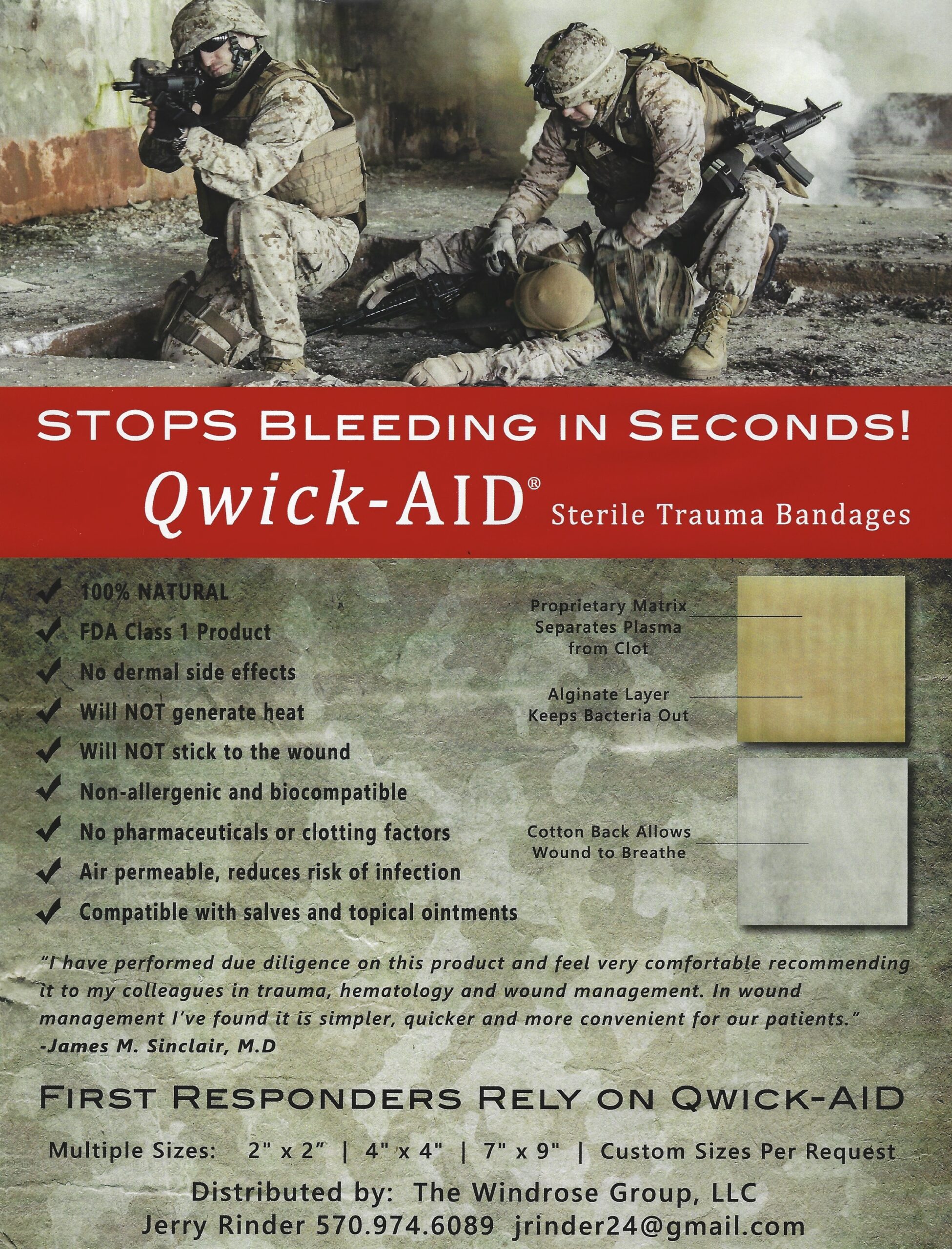
Qwick-AID Bandages are available through The Windrose Group.
Qwick-AID Hemostatic Bandages feature no thermogenic reaction and maintain air permeability. Additionally, the bandage won’t stick to the wound and is hypoallergenic.
Qwick-AID Bandages are available through The Windrose Group.
PATRICK SPACE FORCE BASE, Fla. (AFNS) —
To find a solution to an identified gap in medical care provided in combat situations, the 920th Rescue Wing’s Aeromedical Staging Squadron developed the Tactical Medical Augmentation Team, an embedded medical team that will bring a new level of patient care directly to the battlefield.
This small, multi-capable, highly skilled, and adaptable team of medical personnel can use the wing’s Personnel Recovery Task Force presentation to move higher levels of medical care further forward to wounded warriors and allow pararescuemen and specialty teams to remain closer to the battlespace.
“This capability increases pararescue’s overall mission effectiveness and serves as a force multiplier for combatant and medical commanders in future conflicts,” said Maj. Alexander Torres, TMAT team officer in charge. “It delivers advanced medical care further forward than previous capabilities.”

The concept takes the previously established models of Air Force pararescue, Critical Care Air Transport Team, U.S. Army Dustoff, British Medical Emergency Response Teams and the previous Tactical Critical Care Evacuation Team missions to build a dynamic medical capability that expands the current capabilities of pararescue. By serving as a medical intermediary between pararescue operators and en-route care system, the TMAT concept uses personnel that are already assigned within the rescue wing and is built specifically to cater to the needs of any rescue mission.
The TMAT, as a proposed embedded military rescue community asset, utilizes the PRTF composition of light-, medium-, and heavy-packages to define capabilities. The total team size of a TMAT-Heavy is comprised of six individuals: one physician, two nurses and three paramedics. A medium team is composed of four members: one physician, one nurse and two paramedics. In the light PRTF model, and for maximum adaptability, the team is composed of two members and can be any combination of physician, nurse and/or paramedic depending on mission requirements.
The TMAT-Heavy can provide prolonged field care for 72-hours, the -medium for 48-hours, and the -light for 24-hours. This provides support options when patients can’t be evacuated and need care until transportation is an option or when geographic challenges prevent immediate transport.
The team physicians will be trained in emergency medicine, critical care, anesthesia, or trauma surgery. The nurses will be emergency or trauma trained with trauma and critical care certifications. The paramedics will have advanced training and certification as flight paramedics, thereby providing them with additional critical care and ventilation skills not seen in standard paramedic training.
The team is capable of being utilized on the wing’s rotor and fixed-wing rescue assets as a force multiplier that does not need to rely on transportation outside of the wing. The PRTFs can utilize the land and water assets such as the wing’s Search and Recovery Tactical Vehicles or inflatable boats. Wherever they can get to patients, not only can they provide care, but they can also get them transported on any asset the PRTF can provide.
“Many patient care teams do not have dedicated platforms to evacuate patients,” said Senior Master Sgt. Matthew Harmon, TMAT non-commissioned officer in charge. “By utilizing organic assets in the PRTF, TMAT is able to rapidly bring a higher level of care further forward to patients allowing pararescue to continue to work tactical problems.”
To validate this concept of medical care, the 920th ASTS created a team of six Airmen that developed a lightweight and adaptable equipment allowance and validated its functionality in various transportation platforms. They then completed training with pararescue Airmen in quarterly unit training assemblies and local-level training events. This evolved into placing TMAT light-, medium-, and heavy-packages into wing-level exercises in Florida, Arizona, New Mexico, California, and Hawaii.
A final test of the TMAT’s ability to integrate with the PRTF came during their use in Exercise Balikatan 22, a multinational, joint forces exercise in the Philippines. There they were able to practice these skills within the Indo-Pacific area of responsibility and included a mass casualty exercise, personnel recovery of a downed pilot, and training Filipino pararescuemen in patient assessment and interoperability in a joint environment.
“We believe that TMAT is a valuable asset to the Air Force rescue community,” said Col. Corey Anderson, 920 ASTS commander. “It provides an irreplaceable medical care option that is organic to the PRTF. I’m proud that this team is getting patients the care they need as soon as possible on the battlefield and allowing the pararescue community to stay where they need to be, which is in the fight.”
By Lt. Col. Ian Phillips, 920th Rescue Wing Public Affairs

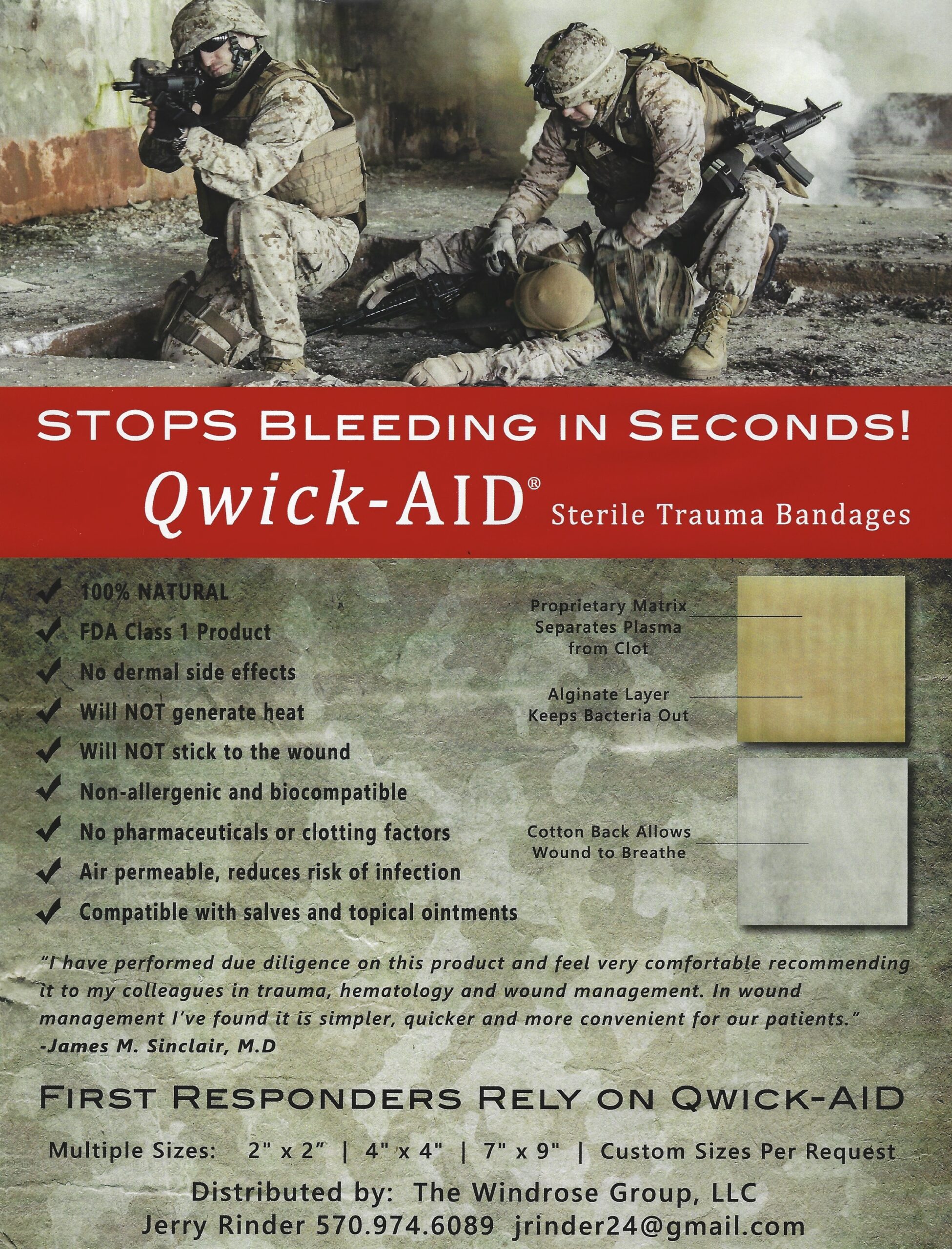
Snakestaff Systems is proud to announce the Everyday Carry Tourniquet (ETQTM). Made in the U.S.A., it’s the smallest and lightest windlass tourniquet on the market. We spent years in R&D developing a reliable tourniquet that is 65% smaller than the industry standard. It fits in most 9mm pistol magazine carriers, in just about any pocket, or even on a keychain.

Responsible citizens are statistically more likely to use a tourniquet than their everyday carry pistol; however, very few people carry a tourniquet. Most tourniquets are large and bulky, making them difficult or uncomfortable to carry on your person. We set out to fix that problem without sacrificing reliability.

The ETQ is packed with innovative features that solve common issues. Occasionally, tourniquet windlasses become displaced during emergency transportation. On the ETQ, a carabiner gate locks in the windlass making the tourniquet more secure. The ETQ also includes a chemlight that automatically snaps and activates when applied—a feature that helps first responders locate an injury in low light. Lastly, the ETQ’s windlass is extremely rigid and textured for positive retention and grip, even when coated in blood.
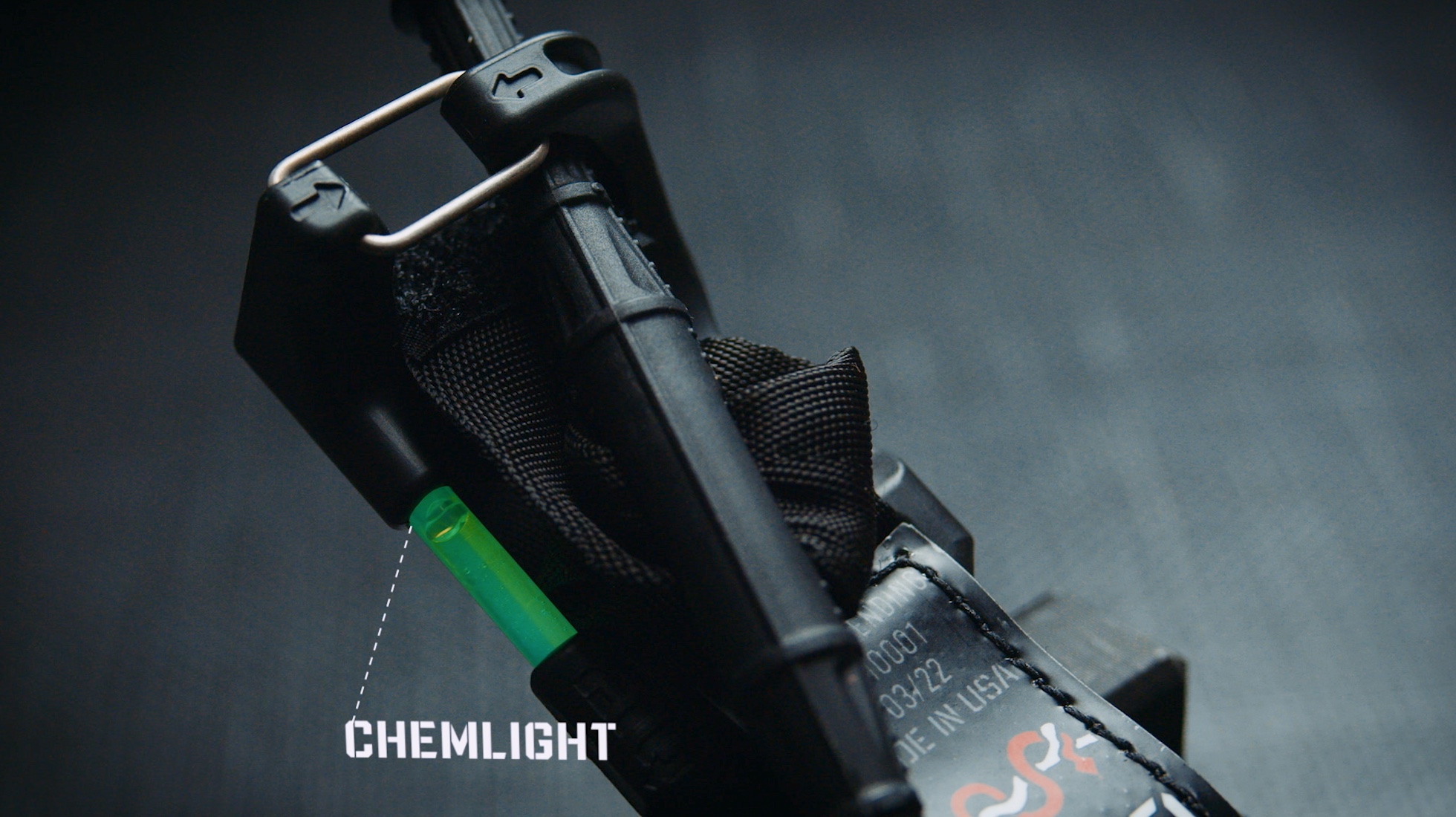
In our research, we found many civilians don’t know the proper way to apply a tourniquet. The ETQ has simple instructions printed on the product, along with a QR code that navigates the user to an easy-to-understand video tutorial. This video can successfully guide someone with zero medical experience through emergency tourniquet application.
For Law Enforcement, Emergency Medical Services, Military, and whoever wants it, we also make the 1.5” ETQ WideTM version designed to meet criteria set forth by the Department of Defense Tourniquet Working Group. We look forward to submitting samples to CoTCCC and continue gathering real world data for when they conduct their next round of TQ evaluations. (Unfortunately they do not meet every year to recommend new TQ’s on the market. The last recommendations were in 2019) This true 1.5” wide version is a little bit easier to use, but slightly larger, at 50% the size of the industry standard.

We have nothing but respect for other tourniquet manufacturers. They have saved countless lives. The ETQ is just another tool in your arsenal. Think of it as a concealed carry handgun – useful when space and concealment is a factor. If you love your current tourniquet brand, keep using it; we just encourage you to carry one everyday, to train with it regularly, and only buy quality American made products.
Your family and friends count on you. Don’t be the guy without a tourniquet in an emergency.
Available for purchase now at: snakestaffsystems.com
WESTPORT, CT (October 26, 2022) – The Q-Collar is an FDA-authorized, non-invasive device intended to be worn around the neck of athletes aged 13 years and older during sports activities to aid in the protection of the brain from effects associated with repetitive sub-concussive head impacts. In an effort to evaluate the safety, effectiveness, and field suitability of the Q-Collar to help prevent or reduce traumatic brain injury (TBI) from blunt force and blast waves in soldiers in the operational environment, Q30 Innovations has been awarded a $2.8 million contract by the United States Army Medical Research and Development Command (USAMRDC).

There were 454,000 diagnosed TBIs in the US military from 2000 through 2021. The United States Army Medical Materiel Development Activity’s Warfighter Brain Health Project Management Office is leading the effort and is now partnered with Q30 Innovations to ensure an advanced solution to help prevent or reduce the severity of TBIs caused by pressure waves from missiles, ballistics, artillery, IEDs, and shoulder-fired weapons.
The Q-Collar is the result of 10 years and more than $30 million in research and development, including independent clinical trials involving hundreds of high school athletes, used to support the FDA-granted De Novo classification for marketing of the device. The Collar is gaining acceptance among premier athletes at the high school, collegiate and professional levels, in sports ranging from football, lacrosse and soccer to bobsledding and surfing; to aid in the protection of the brain from effects associated with repetitive sub-concussive head impacts. The awarded contract enables further research and development to study the safety, efficacy, and field suitability of the Q-Collar in operational scenarios to include blast.
“Q30 is committed to protecting our brave armed forces and we are honored to be a part of the next steps in significantly reducing TBI throughout our military,” said Q30’s Co-CEO Tom Hoey. “The Q-Collar is a proven device to help mitigate the risks of brain injuries caused by head impacts. By working with our DoD partners, we aim to make a direct impact in the lives of our American servicemen and women and their families. We are proud to have been awarded this contract following a competitive bidding process. We are confident that the Q-Collar is the right solution to help protect soldiers who are at risk of TBIs.”

The current contract will advance the research and development of the Q-Collar to prove that it can help reduce blast-induced TBI and that it is a safe, effective, and durable option for soldiers. The funding was made possible because of a congressional mandate to research novel methods to reduce TBI in soldiers.
On the sports field and potentially the battlefield, the Q-Collar is protective gear specifically designed to help safeguard the brain. While a helmet protects the skull from the outside, the Q-Collar gives an added layer of protection on the inside by limiting brain movement. The rapid acceleration and deceleration movement of the brain (commonly known as “brain slosh”) can occur in a number of military situations, leading to the twisting and tearing of neurons, causing traumatic brain injuries.

More information on the product, research, and how to purchase the Q-Collar can be found at q30.com/pages/military.
Garmin has introduced the Index, a blood pressure monitor with a built-in display.

However, the data can also be shared via the Garmin Connect app. It is FDA-cleared and will store readings onboard for up to nine months (limited by battery). You can take a single reading or set the Index to take three readings in a row to provide an average.
As part of long-standing, ongoing efforts to be better prepared to save lives following radiological and nuclear emergencies, the U.S. Department of Health and Human Services is purchasing a supply of the drug Nplate from Amgen USA Inc; Nplate is approved to treat blood cell injuries that accompany acute radiation syndrome in adult and pediatric patients (ARS).
Amgen, based in Thousands Oaks, California, developed Nplate for ARS with support from the Biomedical Advanced Research and Development Authority (BARDA), part of the HHS Administration for Strategic Preparedness and Response (ASPR), as well as the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health.
BARDA is using its authority provided under the 2004 Project Bioshield Act and $290 million in Project BioShield designated funding to purchase this supply of the drug. Amgen will maintain this supply in vendor-managed inventory. This approach decreases life-cycle management costs for taxpayers because doses that near expiration can be rotated into the commercial market for rapid use prior to expiry and new doses can be added to the government supply.
ARS, also known as radiation sickness, occurs when a person’s entire body is exposed to a high dose of penetrating radiation, reaching internal organs in a matter of seconds. Symptoms of ARS injuries include impaired blood clotting as a result of low platelet counts, which can lead to uncontrolled and life-threatening bleeding.
To reduce radiation-induced bleeding, Nplate stimulates the body’s production of platelets. The drug can be used to treat adults and children.
Nplate is also approved for adult and pediatric patients with immune thrombocytopenia, a blood disorder resulting in low platelet counts. Repurposing drugs for acute radiation syndrome that also are approved for a commercial indication helps to sustain availability of the product and improves healthcare provider familiarity with the drug.
The Army Public Health Center has released a preventative health guide for those deployed to disaster response in areas hit by hurricanes.
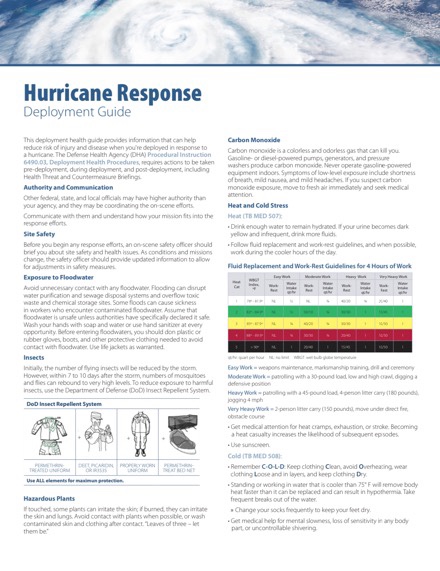
Get yours here.