
What do you think of this potential Strike Industries BIC Lighter sleeve/case from Strike Industries? They are trying to keep it under $10 MSRP each.
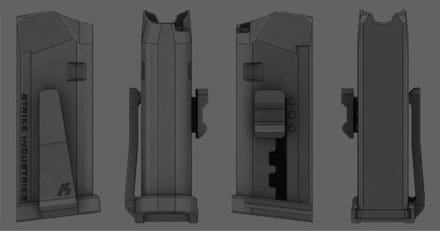

What do you think of this potential Strike Industries BIC Lighter sleeve/case from Strike Industries? They are trying to keep it under $10 MSRP each.
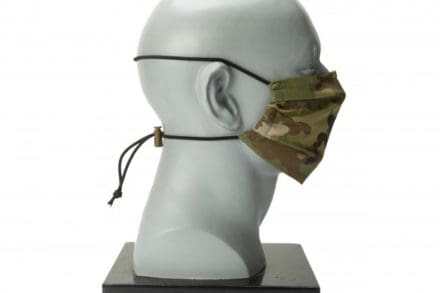
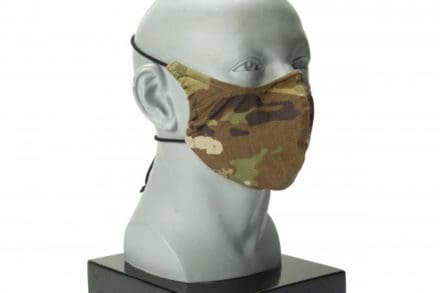
NATICK, Mass. – Dangerous times call for quick action, including rapid prototype development. With this reality in mind, the Combat Capabilities Development Command Soldier Center quickly designed face covering prototypes that comply with Department of Defense standards and meet Centers for Disease Control and Prevention requirements for protection against COVID-19, the disease caused by the Coronavirus.
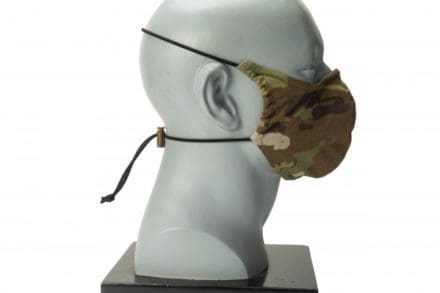
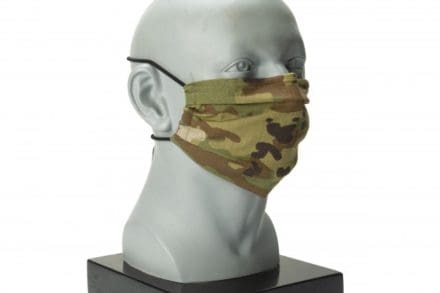
The CCDC Soldier Center, or CCDC SC, quickly developed six prototypes for face coverings, tested the prototypes, and chose one prototype that was highly rated by Soldiers for immediate development. CCDC SC also selected a second prototype, also well received by Soldiers, that has been further developed, coordinated with PEO Soldier, and will be a more permanent Army solution.
CCDC SC efforts focus on the research, development, and early engineering of the solution and building a Technical Data Package. The designs developed at CCDC SC have transitioned to its partners at PEO Soldier – Project Manager Soldier Survivability for production efforts. CCDC SC is also partnering with PEO Soldier on future iterations.
“During the pandemic, we must ensure that our Soldiers remain ready for any mission and that they are protected” said Douglas Tamilio, director of the CCDC SC. “Our Soldier protection and human factors expertise, combined with our testing and prototyping capabilities, enabled us to quickly develop an Army acceptable solution to the urgent requirement for face coverings.”
CCDC SC is committed to discovering, developing, and advancing science and technology solutions that ensure America’s warfighters are optimized, protected, and lethal. CCDC SC supports all of the Army’s Modernization efforts, with the Soldier Lethality and Synthetic Training Environment Cross Functional Teams being the CCDC SC’s chief areas of focus. The center’s science and engineering expertise are combined with collaborations with industry, DOD, and academia to advance Soldier and squad performance. The center supports the Army as it transforms from being adaptive to driving innovation to support a Multi-Domain Operations Capable Force of 2028 and a MDO Ready Force of 2035. CCDC SC is constantly working to strengthen Soldiers’ performance to increase readiness and support for warfighters who are organized, trained, and equipped for prompt and sustainable ground combat.
Annette LaFleur, team leader for the Design, Pattern and Prototype Team in the Soldier Protection and Survivability Directorate at CCDC SC, explained that CCDC SC “designers quickly brainstormed, sketched, patterned, and fabricated prototypes in one weekend – while material scientists, textile technologists and engineers coordinated the test and evaluation of potential materials.”
“The materials selection was a collection of past and current clothing development efforts, as well as sourcing readily available materials from industry,” said Molly Richards, a research chemical engineer at CCDC SC.
LaFleur explained that clothing designers on the Design, Pattern, & Prototype Team worked with load carriage experts at CCDC SC to rapidly develop an array of potential prototype systems that included six potential designs. CCDC SC’s Human Factors Team assessed the prototypes on Human Research Volunteers stationed at CCDC SC. The designs were given to Soldiers for feedback, a key component of all design efforts at CCDC SC.
“CCDC SC items, including the face covering, are developed with the Soldier from the beginning stages, so we can say it is ‘Soldier tested and Soldier approved,’” said Richards.
“The design selected needed no improvements,” said LaFleur. “We down selected to designs with the highest Soldier acceptance while considering other factors such as integration with helmets and eyewear as well as ease of manufacturing.”
The first design developed by CCDC SC is being fabricated in-house. CCDC SC specializes in prototype creation and is not a production shop. However, due to unprecedented circumstances caused by the pandemic, CCDC SC personnel are fabricating the first design, which was chosen because of its high acceptance with Soldiers and because it is easy to produce.
Richards explained that a small team of employees across three directorates are busy fabricating the first design with an initial quantity of 10,000 face covers to outfit Soldiers in basic training at Fort Benning, Georgia.
A second design, also highly accepted, has been further developed rapidly as a more permanent Army solution.
CCDC SC knowledge and expertise played an important role in the rapid design and development of the face coverings.
“We have a team of 10 talented clothing designers who work daily to design new and/or improved combat clothing, uniforms and individual protective items,” said LaFleur. “They have the military specific knowledge, skills, ability and creative drive. We collaborated with other CCDC SC subject matter experts in materials/textiles, human factors, anthropology for sizing; engineering technicians in the machine shop; and so many others in various disciplines. We need our Soldiers to remain healthy so they can remain optimized and defend our nation. At CCDC SC our priority is for the Soldier to not to be burdened by what they are wearing, so they can focus on their mission. For the face coverings, the goal is to meet the intent of the CDC and DOD guidelines for use of cloth face coverings when in public.”
“This effort was a natural fit for the expertise in the Soldier Protection and Survivability Directorate,” said Richard Green, Ph.D., director of SPSD at CCDC SC. “We have expertise in materials that enabled smart choices on the selection of materials to ensure the safety of the users. We have expertise in design to make sure that the items fit, function, and durability are appropriate for the intended use, and we have the expertise to provide our PM partners with technical data packages for further production. Mainly, however, we have a dedicated team of true professionals who were willing to come to work under restrictive working conditions and speedily execute this project because they understand the importance of meeting this need expeditiously. I could not be prouder of their effort.”
“CCDC Soldier Center has the expertise from design and prototyping to materials and textiles to react and execute quickly for the need for face coverings for the Soldier,” said Richards. “It has taken a team of people across directorates with a variety of expertise to execute quickly. Protection for our Soldiers is our top priority and taking measures to limit the spread of COVID-19 is essential during this unprecedented time.”
JOINT BASE ELMENDORF-RICHARDSON, Alaska
Two 673d Medical Support Squadron (MDSS) Airmen refined their invention of a plastic barrier to protect medical providers treating patients with COVID-19, and airborne diseases in general, at Joint Base Elmendorf-Richardson, Alaska, April 7, 2020.

U.S. Air Force Senior Airman Michael Shoemaker, 673d MDSS biomedical equipment technician, and U.S. Air Force Staff Sgt. Andrew Taylor, 673d MDSS medical logistics noncommissioned officer in charge of acquisitions, designed and built a polycarbonate plastic enclosure to place over a patient’s head and upper torso with access for treatment via two holes at the head of the enclosure for a physician’s hands and arms, and two side doors for additional access.
“Ultimately, we wanted to create a mobile isolation room that could contain an infectious disease,” Shoemaker said. “This enclosure provides an extra layer of protection for medical staff because aerosol droplets can’t pass through it.”
Shoemaker said he got the idea after seeing the large, bubble-like ventilators medical providers in Italy and New York were using to treat patients with COVID-19. The ventilators had sufficient space around a patient’s head for a physician to reach inside and treat the patient from outside the barrier.

Shoemaker shared his idea for a sturdy, plastic barrier that could surround a patient’s head and upper torso with MDSS leadership, using a cardboard box for a visual. He said his leadership immediately gave him the go-ahead to build a prototype, and Taylor came on board to help with supplies and construction.
Taylor and Shoemaker built an acrylic prototype that same day, then invited medical professionals from infection control, respiratory therapy and anesthesiology to provide feedback and suggestions for improvements. A paramedic also intubated a medical manikin under the enclosure to assess its practicality.
“It was really cool to see the whole team excited about the idea, looking at the capability it could provide,” Shoemaker said. “Everybody was onboard. They pointed out shortfalls in the initial design and what we needed to change. For example, curving the front so there wasn’t a seam on the viewing platform, and making sure there were doors on the sides so medical technicians could support the physician.”

“Their recommendations made this enclosure a lot more functional than we originally anticipated,” Taylor said. “It could be used for more than the current situation with COVID-19. It could be used for almost any medical procedure needing an extra barrier for protection.”
To create the enclosure, polycarbonate plastic panels are cut with a waterjet, so they fit together almost like a puzzle. Thin brackets and rivets secure the panels together, and clear silicone seals the seams. The team is also working to create a single panel that can be folded into shape using heat, eliminating the need for brackets and rivets.
“It’s simplicity allows it to be quickly cleaned and sterilized after each use and ready for another patient in five to 10 minutes,” Taylor said.
“Working with the base innovation lab and the staff at the medical group, we’ve created something significant,” Shoemaker said. “If this is adopted and we’re able to make this a kit that can be sent out, it will outlast COVID-19 and go to any medical group with a need for it.”

In less than a week, with help from the 673d Medical Group, the JBER Innovation Lab and support from across the installation, these two Airmen created a functioning, potentially life-saving device.
By Airman 1st Class Samuel Colvin | 673 ABW/PA
ADELPHI, Md. — As the world confronts the shortage of essential medical equipment caused by the COVID-19 pandemic, the internet buzzes with efforts to build makeshift ventilators, some based on the idea of a respirator invented by U.S. Army researchers more than five decades ago.
When the coronavirus epidemic began to strain the supply of lifesaving medical equipment like ventilators, online communities of technologists banded together to help small companies and even everyday people create their own emergency medical equipment.
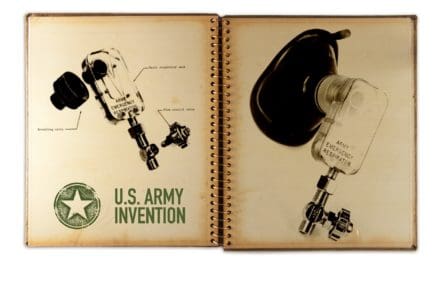
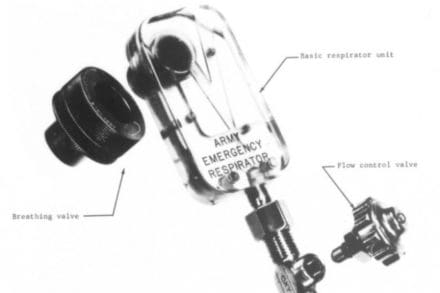
Among the many ideas and personal projects shared on internet forums, many people got excited over the design of a unique ventilator known as the Army Emergency Respirator. What caught their attention about this technology was that this particular apparatus could perform complex breathing-supporting functions without the need for any moving parts.
The Army Emergency Respirator has two configurations; a respirator with a moving bellows that takes over the intubated and sedated patients breathing, and a simple breathing assist device to help the patient breathe easier through pressure augmentation.
Army engineer Henrik H. Straub invented the device in 1964 while he worked at the Harry Diamond Laboratories, one of the seven facilities that merged to form the Army Research Laboratory in 1992.
The respirator represents one of the many important scientific milestones in the history of the U.S. Army Combat Capabilities Development Command’s Army Research Laboratory, officials said. It uses the principles of fluidics to assist or control the ventilation of the patient.
“The fluidic breathing assist device relies on the person’s labored and insufficient breathing to control the fluidic augmentation of breaths using a power-jet directed into or away from the patient’s face mask,” said Michael Scanlon, a branch chief with the lab. Scanlon began his career in the development of fluidics technology about 37 years ago when he started as a Cooperative Education student at Harry Diamond Laboratories.
Based on the theoretical foundation of fluid dynamics, fluidics allows a system to operate under a control comprised of pipes and other pneumatic or hydraulic components. Much like how electronic circuit boards use wires and electronic valves to direct the movement of electrons and govern the system’s functions, fluidic devices use small jet streams that travel along a circuit board-like structure to perform analog and digital operations. Depending on how a fluid circuit is arranged, engineers can create a variety of machines controlled entirely by the flow of liquid or gas traveling down carefully designed paths.
At the time, Harry Diamond Laboratories received a great amount of attention for pioneering the study of modern fluidics with the invention of the fluid amplifier in 1957, a device that forces a stream to follow a designated path and amplifies its power.
The apparatus named at the time the Army Emergency Respirator emerged as just one of many applications of this new breakthrough in fluidics. The device was developed by Straub and his collaborators at the Walter Reed Army Institute of Research to mainly function as an inexpensive yet reliable pressure-cycled respirator for when supplies run low.
The breathing assist device connects to a breathing mask and automatically helps the patient inhale and exhale with a feedback loop that takes advantage of the changing pressures inside of the mask.
When the air pressure inside the breathing mask is lower than outside the mask, the apparatus pulls in air from outside through a nozzle and carries oxygen into the patient’s lungs. Then, once the pressure inside the mask increases to a preset point, the apparatus automatically adjusts to help the patient to exhale, sending the air out through a different nozzle.
As a fluidic device, Straub’s invention didn’t require any moving parts. In fact, the laboratory’s prototype was only slightly larger than a pack of playing cards and consisted of a Lucite block with a system of intricate channels carved inside. However, its relatively simple design meant that it serviced as a low-cost disposable tool for routine use at hospitals and clinics.
“The elimination of moving parts in the respirator itself makes this device extremely reliable, easy to operate, and inexpensive to manufacture,” Straub stated in one of his 1965 reports.

While Straub successfully tested his pressure-cycled respirator on dogs and human patients, the device remained in development as a working prototype and was never fully fielded by the U.S. Army. A similar model called the Fluidic Breathing Assistor was patented by the Bowles Fluidic Corporation in 1971, but Army research into the apparatus discontinued by the 1980s.
Despite having been confined to history for over 50 years, the renewed public attention surrounding Straub’s invention gained momentum in last few weeks as independent technologists realized its potential – and discussed it on the internet – during this time of pandemic.
One engineer has already constructed an updated version of the 1965 ventilator and shared a video of the finished product on the social media website Reddit, prompting other users to look into the design as well.
“These fluidic designs [like those featured in Straub’s pressure-cycled respirator] are so simplistic that they are suitable for mass production at negligible unit cost,” Scanlon said. “Additive manufacturing technology, such as 3-D printing with plastics, will likely enable research prototypes to be quickly and inexpensively built and tested.”
The longevity of this one invention demonstrates how foundational knowledge created within the Army laboratories can lead to an impact that extends far beyond its originally envisioned applications, and over multiple decades, officials said.
Disclaimer: The U.S. Army Combat Capabilities Development Command’s Army Research Laboratory does not approve nor recommend any medical devices and has no position on any proposed applications of the Army Emergency Respirator for any purposes.
By U.S. Army CCDC Army Research Laboratory Public Affairs
Soldiers at Fort Pickett, Virginia are testing a Microsoft-designed prototype goggle, the Integrated Visual Augmentation System (IVAS). New technology offers capabilities that troops need to regain and maintain over-match in multi-domain operations on battlefields that are becoming increasingly complex and unpredictable.
US Army video by Mr Luke J Allen
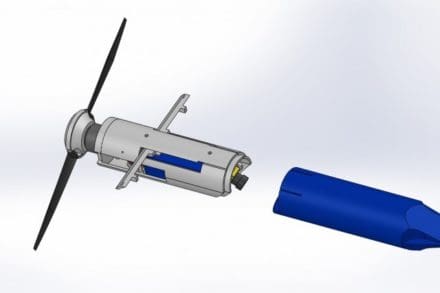
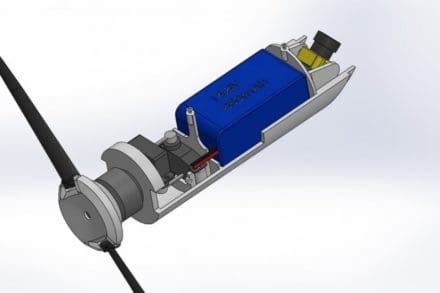
ABERDEEN PROVING GROUND, Md. — Scientists from the Army Research Laboratory have designed a camera drone capable of being fired from a 40 mm grenade launcher, researchers say, on the heels of a patent filed last month.
There are two variants of the Grenade Launched Unmanned Aerial System, or GLUAS, one is a is a small, paragliding system with folding blade propellers and Mylar paragliding wings to help it stay in the air, and the other is a helicopter-style that hovers on a gimbaling set of coaxial rotors, said John Gerdes, a mechanical engineer with ARL.
The GLUAS is a small projectile, 40 millimeters in diameter, can cover a long distance with a gun-launching system. The breakthrough, he said, is with how miniaturized autonomous flight hardware has become.
The drone has a 2-kilometer range with a projected battery life that could top 90 minutes, and is capable of operating up to 2,000 feet in the air, according to researchers.
After launching, the drone spreads its wings and soars at a fixed airspeed controlled by ground troops with a joystick or handheld device. On the drone, a camera is equipped to provide a video feed to a ground station below.
“In battle, there are multiple scenarios of when Soldiers would use this technology,” Gerdes said. “How it’s used depends on which theater they’re operating in.”
For example, on the mountain ranges of Afghanistan, if Soldiers found themselves under sniper fire, they could deploy the drone to check over the area and determine the enemy’s location.
The lightweight GLUAS drone is designed to increase Soldier lethality by giving them a bird’s eye view of the battlefield, he explained, and will easily integrate into most kits carried by Soldiers in the field.
“This device provides an autonomy and intelligence platform to help Soldiers perform useful missions while having a lookout from hundreds of feet in the air,” Gerdes said. “This integrates modern types of intelligence.”
“[GLUAS] is aligned with Army modernization priorities,” said Hao Kang, another mechanical engineer with ARL. “We’re trying to provide capabilities to individual Soldiers. The most exciting part of this is the viability of this platform, coupled with its gun-launched deployment capabilities.”
“Things like GPS receivers and flight controllers are very feasible to install [onto the GLUAS], which makes it easy to maintain a position or follow a ground unit,” Gerdes said. “Basically, if there is something you want to look at, but you have no idea where it is yet, that’s where the drone comes in.”
Although they’re making technological breakthroughs at ARL, the scientists aren’t working on the same timelines as other developers, Kang said.
“We’re here to develop innovative concepts for the warfighter’s needs, which generally means we bring the size and weight down of a device, and push up the range and lethality,” Gerdes said. “At ARL, we’re typically focused on the basic innovation and discovery aspects of research.”
ARL is part of the Combat Capabilities Development Command. As the Army’s corporate research laboratory, ARL discovers, innovates and transitions science and technology to ensure dominant strategic land power.
By Thomas Brading, Army News Service
The Army is supporting the nation’s fight against the COVID-29 pandemic which is led by FEMA. One of their initiatives is the xTech COVID-19 Ventilator Challenge which seeks a low-cost, readily manufacturable emergency ventilator to quickly augment ventilator capacity during the COVID-19 pandemic. The technology solution must provide a rapid response breathing apparatus capable of short-term, rugged field operation.
The prize competition will evaluate technology proposals immediately upon submission and award novel solutions with a prize of $5,000 to present a virtual pitch of the technology concept to the xTech COVID-19 panel, and award prizes of $100,000 to solutions accepted by the panel to develop a concept prototype. Select technologies may receive follow on contracts for additional production and deployment.
The total prize pool is $1,000,000.00.
• Application Part 1: White Paper – $5,000
• Application Part 2: Technology Pitches – $100,000
Virtual pitches for selected companies will begin April 13.
Details here.
Submit here.
xTechSearch is a competition sponsored by the Assistant Secretary of the Army for Acquisition, Logistics andTechnology (ASA(ALT)), targeting small businesses.
GOODFELLOW AIR FORCE BASE, Texas (AFNS) —
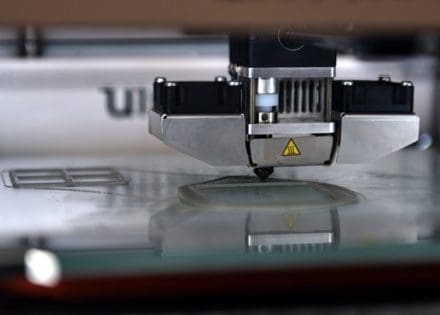
The 312th Training Squadron’s Special Instruments Training course instructors have begun using their skills to 3D print prototypes to supply the medical facilities in the area with N95 face masks and face shields.

A neurosurgeon in Billings, Montana, worked with a dental company to create reusable plastic N95 masks using 3D printers. In an effort to help protect those caring for sick individuals around the world, he made a model available online for a free 3D printable, high-efficiency filtration mask with a design that allows reuse of the mask several times due to the replaceable filtration device.

U.S. Air Force Tech. Sgt. Donald Kramer, 312th Training Squadron Special Instruments Training course instructor supervisor, cuts the clear, plastic shield for the 3D printed face shields at the Louis F Garland Department of Defense Fire Academy on Goodfellow Air Force Base, Texas, March 31, 2020. Many SPINSTRA instructors have personal 3-D printers home, providing more resources to the project. (U.S. Air Force photo by Airman 1st Class Robyn Hunsinger)
Instructors got the idea from Air Force Quarantine University, a public Facebook group for innovative learners to connect during the COVID-19 crisis, where they saw other organizations modeling and printing these supplies.
“We saw other people 3D printing medical supplies and we thought we should try printing things like face masks and face shields,” said Master Sgt. Manuel Campo, 312th TRS SPINSTRA flight chief.

SPINSTRA has an innovation lab containing four 3D printers as well as 3D modeling software. Although they are unsure of the needs of the 17th Medical Group and surrounding hospitals, they plan to continue to create these medical supplies in case they are needed in the future.
“We plan to present what we have created to the medical group to see if we can meet their needs and print what they need,” said Staff Sgt. Jonathan Bahr, 312th TRS SPINSTRA instructor.

Medical professionals wear personal protective equipment to protect themselves and minimize exposure. This PPE usually consists of a face mask, gloves, and goggles or a face shield.

“The most realistic option for us to make was the face shields,” Bahr said. “The purpose of the face shield is to extend the use of the face mask. The goal is to reduce the number of masks being used and thrown out after one use.”
In the future, if more masks and shields are needed to be printed, they plan to allow students to begin assisting in this project. Instructors have also reached out to other facilities on Goodfellow AFB with 3D printers to provide more medical supplies. There are even instructors with personal 3D printers providing more supplies from home.
“If we can use our skills to help, we plan to do so,” Campo said. “We want to do everything we can to help.”
By Airman 1st Class Robyn Hunsinger, 17th Training Wing Public Affairs