I grew up in Connecticut and spent a significant amount of time only miles from Lyme, CT where the effects of lyme disease were first detected and reported. As beautiful as Connecticut’s forests, coastlines, and countrysides are, they are breeding grounds for deer ticks not to mention mosquitos, black flies, no-see-ums, and other pests. When I was younger, the only viable option we had was insect repellent with DEET in varying concentrations. The strongest DEET available was used primarily on clothing as it was considered too strong and potentially unsafe. Repellent paired with daily and nightly vigilance was the best answer to the tick and insect problem. Over the years, I used other products that worked with mixed results. Recently, I was exposed to Bullseye Insect Repellent with IR3535. This Department of Defense-approved product was advertised as working better and longer than DEET; a claim I had to test myself. While field testing Bullseye, I reflected on some best practices for repellents like this one. Just like any gear, it isn’t just that we have it, it is how we use it.

Apply and Let Dry
Bullseye comes in a 4 ounce spray bottle and it applies as a mist. In a matter of minutes, the insect repellent feels dry to the touch. Compare this to DEET repellents that have an oily residue after application. Long after you apply DEET, it makes your skin sticky and can rub off on your gear. Bullseye is different. During my field test, I found it very easy to remove my watch, roll up my sleeves, roll down my collar and spray it on. After a couple minutes of double checking my backpack contents or prepping my fishing tackle, I rolled the sleeves down, put my collar back up, and wristwatch back on. The reason Bullseye dries so quickly is because an alcohol is used which evaporates quickly. Once dry, you are free to recreate as you please knowing you have approximately 8 hours until you have to reapply. By the way, one of the bonuses of this dry sensation is sleep. In years past, with DEET, I couldn’t sleep comfortably if I knew I had it on my skin. You can apply Bullseye overnight as long as you follow the same protocols as you would during the day.

Ankles, Waistline, Wrists, Neckline
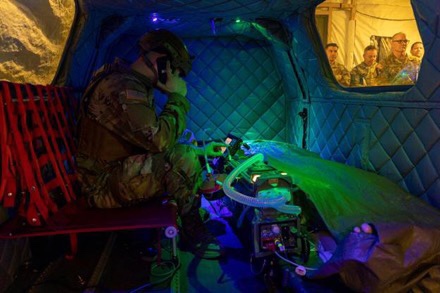
As someone who spends a lot of time at elevation and spends a lot of time on self-supported trips to the backcountry, space and weight are crucial. One of the ways to respect both is to make sure the ounces and pounds you carry are utilized well. With insect repellent, it is easy to go overboard quickly. Instead of creating a fog to pirouette in, be tactful with your application. While in Idaho recently for a training event, I used a single bottle of Bullseye (4 ounces) on my ankles, waistline, wrists, and neckline. These are the typical entrance points for ticks as the ankles are close to the ground, the waistline is warm, and cuffs and collar can lead to the armpits and hairline respectively. I was impressed how far I could stretch a single bottle as long as I rationed it for use in these spots. I used to hesitate to apply deet to my wrists and neckline in particular knowing DEET has potential dangerous nervous system side effects.
Backhand to the Face
Perhaps one of the most annoying habits of mosquitoes and flies is their insistence on flying into your mouth, eyes, and ears. Keep in mind, mosquitoes have special receptors that are attracted to the carbon dioxide we breathe out. One would think applying bug spray to your face would be as simple and straightforward. Traditionally, DEET was used as it was designed to disorient the flying nuisances but once disoriented, there was nothing stopping them from flying directly into you since they had to be close enough to smell it. Keep in mind, this also meant your body had to be exposed to the DEET and the strong chemical smell it gave off. A better option than spraying your face is to apply a better insect repellent like Bullseye to the back of your hand and wipe it on. We use the back of our hand already for wiping sweat from our brow and wiping insect repellent is second nature. There’s a reason you want to use the back of your hand. We touch our face frequently throughout the day. We wipe food from the edge of our lips, we rub our eyes, some of you might pick your nose. Even though the active ingredient in Bullseye, IR3535 is both non-toxic and odorless, you always want to keep the palms of your hands clean. Perhaps one of the most important best practices with bug spray is avoiding cross contamination. We’ve all probably experienced what happens when you accidentally taste something that was meant for external use only like sunscreen or a topical medicine. Some of you may have cooked with spicy peppers and rubbed your eyes. An easy way to avoid getting anything for external use only where it shouldn’t be is to keep the palms of your hands clean.
Help Kids or Those with Limited Mobility
As previously mentioned, I grew up in CT and spent a lot of my youth running around the woods getting cuts and scrapes while having a grand old time like every kid should. Before I would run off to the woodline with my friends, my parents applied a combination of sunblock and bug spray to my exposed skin. I personally would not put DEET on my kid someday but I would not hesitate to use Bullseye. As an able-bodied adult, it is a good idea to help kids and those with limited mobility apply insect repellent. Anyone with an ailing and aging parent knows how caring for them is much like looking after a child. Sometimes you have to do for them what they are too stubborn to do for themselves. When it comes to your kids, apply insect repellent to the palms of your hands and rub it into the skin on their arms, legs, and neck. If you abide by my suggestion to keep your palms clean, wash your hands after applying it to them. No disrespect to Bullseye but good advice is good advice and cleanliness is next to Godliness, right? If your kids are like I was, you will have to call them back in to reapply it after 8 hours and hopefully your kids aren’t ready to go to sleep or stop playing when the street lights flicker on as the sun drops below the horizon.
Application Tips
With any insect repellent, you want to follow instructions carefully but sometimes common sense isn’t included on the packaging. Apply your aerosol outdoors or in a well-ventilated area away from the rest of your gear. Step outside your tent and get out in the open. While the gear we use is often durable and long-lasting, we can never be certain how additional ingredients in it will interact with painted surfaces and polished finishes. Also, just like we want to avoid exposure to our eyes, we also don’t want to breathe in what we don’t have to. This is true of any aerosol spray. When you or the other members of your party are applying it be cognizant of others in your immediate area. Also, keep in mind, if you are involved in any activities around water or those that result in you sweating profusely, the repellent may be removed as a result. Also, remember that a little will go a long way and it isn’t wise to overdo it. Since it is fragrance free, you may not think it is present but it is and you don’t need to reapply. Keep in mind a repellent like Bullseye works by shielding your carbon dioxide and it’s more important to create a schedule of 3 applications in an 8 hour day than when you perceive more insects present.
Highest Recommendation
As a survival instructor, I am often asked, “how do you deal with ___?” or “what’s the best solution to ____?” Often, these questions pit man against nature. So far, nature has an unbeaten track record. Without supplies, we are ill equipped to run faster than most predators, we can’t see in the dark, and we are poorly insulated against the cold. We must use our intellect to create, acquire, and equip ourselves with gear that provides an advantage to us over our environment. I’m a firm believer in carrying the best gear I can afford and what makes the most sense. I’ve used DEET products in the past as well as citronella candles and various electronic repellents but I’m certain Bullseye is far superior to anything I’ve used in the past. Bullseye has impressed me with its ability to prevent bites from the pests I learned all too well about in my childhood. It is my job to teach skills that mitigate risk when we get the opportunity to explore the great outdoors but I also advocate for ways to live a healthy life from one day to the next. This includes not using products that could potentially negatively impact someone’s way of life. I’ve done the research on this one and I’ll recommend you equip yourself with it to gain an advantage, 8 hours at a time, in the worst buggy environments. Bullseye is the best, being tough on insects and gentle on skin. It is exactly what is needed to get the most out of your outdoor adventures.
How to Purchase Bullseye:
If you’d like to purchase Bullseye Bug Repellent there are 2 options, eBay: www.ebay.com/itm/165091832029
Website: litefighter.com/product/bullseye-bug-repellent
By: Kevin Estela
About the Author:
Kevin Estela is the best-selling author of the book 101 Skills You Need to Survive in the Woods as well as hundreds of published and online magazine/website articles. He is a professional survival instructor with over 2 decades of outdoor education experience. Kevin is an avid traveler, outdoorsman, athlete, and adventurer. He has dozens of appearances on podcasts, at trade shows, and industry events speaking on readiness, mindset, training, and gear. He is frequently tapped to test, evaluate, and design equipment and has produced a wide variety of content across multiple social media platforms. Follow Kevin on Instagram @estelawilded | estela@fieldcraftsurvival.com